I’m so excited to be freezing my eggs! What a funny thing to be announcing but it’s a big deal for me for a couple of reasons: 1) I’ve been wanting to do this for years but never really prioritized it and 2) Talking about fertility and bringing more awareness to it is so important to me.
So why now? After I was diagnosed with kidney cancer last year, I took a look at what was in my life and what I really needed in it. It wasn’t a closet full of clothes, it wasn’t a fancy car. Everyone has different priorities but for me, I always knew I needed kids in my life.
Most aspects of my life have been fluid and ever-changing but ever since I can remember, I knew that I wanted to have children. However, just because I want them does not mean that I can have them right this very moment. I went through my list of options, adopting, trying naturally – and both don’t currently align with my life structure. So freezing my eggs, for me, seemed to be the natural fit.
I look at freezing my eggs as essentially freezing time. So if in 5 years, I’m in a situation in life where I am ready to have children but am unable to get pregnant naturally, I can try using my “younger” eggs that I’ve frozen at this time in my life.
I wanted to dive into some basics around egg freezing. I’m not a medical professional but I do know some basics especially after talking with my medial team at CCRM and I wanted to share these with you.
Why is freezing your eggs important?
As we age, we have a natural decline in our eggs; therefore, our fertility.
Women are born with as many eggs as we’ll ever have in life.
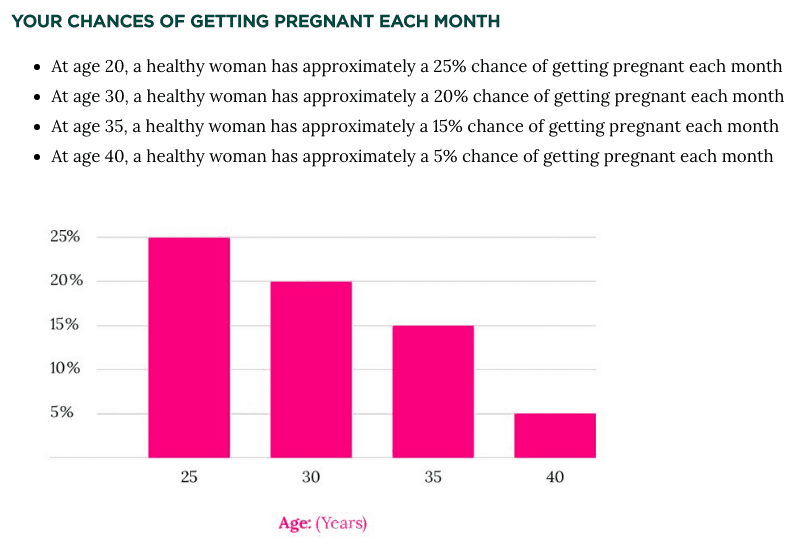
So when we’re born, we have as many as 1,000,000-2,000,000 eggs. Then, once we hit puberty that number can go to around 300,000 eggs. And from there, each month we gradually lose eggs. The graph below gives you a sense of how likely it is to actually get pregnant as we age – for a “healthy” woman.
For me personally as my X axis was inching closer to the right, I decided to reach out to CCRM – Colorado Center for Reproductive Medicine to begin this part of my journey.
What happens at your first visits?
The first step that you take when going into the CCRM office in Lone Tree, Colorado, is you get a consultation with the doctor. I happen to be seeing Dr. William Schoolcraft who is actually a founder of CCRM! Here, the doctor will talk to you about your options, what to expect in the process, and make sure this is the path you want to go down.
I had the option to think about it but I know this is what I want so I chose to get my ultrasound and lab work done during this same visit.
The CCRM location in Lone Tree is really large; however, the systems they’ve got in place there don’t make you feel aimless. I felt so taken care of which, for me, is so important when choosing a doctor who is going to be a part of such a personal part of my journey. Once you check in and see the doctor, you are assigned a primary nurse who will be your main point of contact. This nurse will walk you through the whole process again except in more detail. She’ll let you know exactly what is coming up for you. Plus it’s her chance to ask you some questions about your medical history and your cycle. A medical first date, if you will, to get to know some basics.
After you see the nurse, you’re then either taken to do blood work or get an ultrasound done.
There are 3 important steps to the “initial” phase. What’s important to note is that while these tests can test for potential quantity they cannot test for the quality of your eggs.
First: Checking your AMH levels
What is AMH?
AMH stands for Anti-Mullerian hormone. It’s a hormone that is produced in the ovaries by tiny early-stage follicles as they grow to a stage where they can potentially produce eggs for ovulation. AMH levels can provide an estimate of whether or not there is still a significant number of growing follicles.
It is the most sensitive marker for ovarian reserve and does not fluctuate significantly during or between your menstrual cycle.
Second: Hormone testing for FSH, LH, E3 levels
These hormones must be timed with day 2 or day 3 of your menstrual cycle, as the levels can fluctuate between cycles. These are blood tests to check your ovarian reserve. In other words, checking your fertility level.
Third: Baseline ultrasound
The movies suggest all ultrasounds are done by putting jelly on your belly. Nope! Not this one! Haha it’s a transvaginal ultrasound where a probe is inserted into your vagina so that the ultrasound technician can see your uterus, ovaries, and count how many follicles you have. It’s perhaps a little uncomfortable but generally painless and over in a few minutes, so don’t worry.
Immediately after the ultrasound, you can ask the technician how many follicles were seen and if there was anything abnormal. For me, I had 17 follicles and fortunately nothing came up that was alarming. That follicle count is apparently normal for someone in their mid 30s.
Once the doctor has all of this information, he is able to provide you a protocol that is specific for you. A protocol is essentially the step-by-step guide to how to proceed further in terms of how much and what medication.


























show comments